Covid 19 isnt over how to stay safe – COVID-19 isn’t over: How to stay safe in a world that’s still grappling with the virus. While restrictions have eased, the threat of COVID-19 lingers, with new variants emerging and long-term health effects becoming increasingly clear. This isn’t about fear-mongering; it’s about informed protection. We’ll break down the current situation, explore effective prevention strategies, and help you navigate the ongoing pandemic with confidence.
From understanding the latest variant information and the importance of vaccination to mastering hygiene practices and knowing when to get tested, we’ll equip you with the knowledge to protect yourself and your loved ones. We’ll also tackle common misconceptions and point you towards reliable sources of information, cutting through the noise and empowering you to make informed decisions about your health.
Understanding the Ongoing Threat of COVID-19
COVID-19, while no longer dominating headlines as it once did, remains a significant global health concern. The virus continues to circulate, evolving into new variants and leaving a trail of long-term health consequences. Understanding the current landscape is crucial for informed decision-making and proactive protection.
The global situation regarding COVID-19 is characterized by ongoing circulation of the virus, albeit at fluctuating levels depending on geographical location and implemented public health measures. While many countries have transitioned to a “living with COVID” approach, new variants continue to emerge, posing potential challenges to existing immunity and requiring ongoing monitoring. The impact varies regionally, with some areas experiencing significant surges in cases while others maintain lower levels. This dynamic situation necessitates a continued, cautious approach.
Long-Term Health Effects of COVID-19
COVID-19 infection can lead to a range of long-term health problems, collectively known as “Long COVID” or Post-COVID-19 Condition. These effects can impact various organ systems and manifest in diverse ways, ranging from persistent fatigue and shortness of breath to cognitive impairment (“brain fog”) and cardiovascular issues. The severity and duration of Long COVID vary significantly between individuals, with some experiencing mild symptoms while others face debilitating conditions impacting their quality of life for extended periods. Research continues to unravel the complex mechanisms underlying these long-term consequences. The precise prevalence of Long COVID remains uncertain, as studies employ different diagnostic criteria and methodologies. However, available evidence suggests that a substantial proportion of those infected, even with mild initial symptoms, may experience lasting health repercussions.
Current Infection Rates and Hospitalizations
Precise, real-time statistics on global COVID-19 infection rates and hospitalizations are challenging to obtain due to variations in reporting practices and testing strategies across countries. Many nations have reduced widespread testing, leading to underreporting of actual case numbers. However, data from various sources, including the World Health Organization (WHO) and national public health agencies, provide a general picture. While overall infection rates have decreased from peak levels, fluctuations are common, often influenced by seasonal factors, the emergence of new variants, and the level of immunity within a population. Hospitalization rates generally correlate with infection rates, although the severity of illness varies depending on factors such as vaccination status, underlying health conditions, and the specific variant circulating. It’s crucial to rely on reputable sources for the most current data, as these figures are dynamic and subject to constant change.
Severity of Different COVID-19 Variants
The severity of different COVID-19 variants has varied throughout the pandemic. While some variants have been associated with increased transmissibility, others have shown alterations in their ability to cause severe illness. Direct comparison is complex, as severity is influenced by numerous factors including vaccination status and prior immunity.
| Variant | Transmissibility | Severity | Notes |
|---|---|---|---|
| Alpha (B.1.1.7) | High | Moderately Increased | Associated with increased hospitalization rates compared to earlier variants. |
| Delta (B.1.617.2) | Very High | Increased | Highly contagious, leading to significant surges in cases and hospitalizations. |
| Omicron (B.1.1.529) and subvariants | Very High | Generally Lower | Highly transmissible but often associated with milder illness compared to Delta, although still capable of causing severe disease in vulnerable individuals. |
| XBB.1.5 and subsequent subvariants | Very High | Variable | High transmissibility and immune evasion capabilities, impact on severity is still under investigation. |
Vaccination and Boosters: Covid 19 Isnt Over How To Stay Safe
The COVID-19 pandemic highlighted the crucial role of vaccination in protecting individuals and communities. While the initial vaccines proved remarkably effective, the emergence of new variants necessitates ongoing adaptation and a deeper understanding of booster shots’ importance. This section delves into the effectiveness of current vaccines, the significance of boosters, global vaccine accessibility, and the overall safety profile of COVID-19 vaccination.
Current vaccines remain a vital tool in mitigating severe COVID-19 illness, hospitalization, and death, even against prevalent variants. While their effectiveness against infection might wane over time, especially with new variants, they continue to provide substantial protection against severe outcomes. This protection is significantly boosted through timely booster shots.
Vaccine Effectiveness Against Variants
The effectiveness of COVID-19 vaccines against various variants fluctuates. Studies have shown that while the original vaccines may offer reduced protection against infection from newer variants like Omicron, they still maintain considerable efficacy in preventing severe disease, hospitalization, and death. This highlights the importance of vaccination, even if complete infection prevention isn’t guaranteed. Data from numerous studies, published in peer-reviewed journals, consistently support this observation. For example, a study published in the Lancet showed that while vaccine efficacy against infection decreased with emerging variants, protection against severe disease remained relatively high.
The Importance of Booster Shots
Booster shots are essential for maintaining a robust immune response against COVID-19. Over time, the immune response generated by the initial vaccine doses can diminish, leaving individuals more vulnerable to infection and severe illness. Boosters act as a “refresher,” significantly increasing antibody levels and strengthening the immune system’s ability to combat the virus and its variants. This is especially important for vulnerable populations like the elderly and those with underlying health conditions. The timing of booster shots is crucial and is typically determined by public health authorities based on emerging variant data and vaccine effectiveness studies.
Global Vaccine Accessibility and Distribution
Equitable access to COVID-19 vaccines remains a significant global challenge. While high-income countries have largely achieved high vaccination rates, many low- and middle-income countries face significant hurdles in vaccine procurement, distribution, and administration. This disparity underscores the need for international cooperation and equitable vaccine distribution mechanisms to ensure global health security. Initiatives like COVAX, aimed at providing vaccines to low-income countries, play a crucial role in bridging this gap, but further efforts are needed to overcome logistical and infrastructural barriers. Examples of successful distribution strategies in various regions can offer valuable lessons and inform future pandemic preparedness efforts.
Infographic: Benefits and Safety of COVID-19 Vaccination
The infographic would feature a visually appealing design, utilizing icons and charts for easy understanding.
Section 1: Benefits: This section would display three key benefits: (1) Reduced risk of severe illness, hospitalization, and death (illustrated with a bar graph comparing hospitalization rates in vaccinated vs. unvaccinated individuals); (2) Protection against long COVID (represented by an icon of a healthy person versus one experiencing fatigue and other long COVID symptoms); (3) Community protection through herd immunity (depicted with a visual of interconnected people, representing the protective effect of widespread vaccination).
Section 2: Safety: This section would address safety concerns: (1) A list of common, generally mild side effects (e.g., soreness at injection site, fever, fatigue), emphasizing their temporary nature. (2) A statement reassuring readers that rigorous safety testing was conducted before vaccine approval, citing examples of regulatory bodies involved (e.g., FDA, EMA). (3) A clear message that serious side effects are extremely rare, highlighting the benefits far outweighing the risks. (4) A clear contact point for reporting any adverse effects.
Hygiene Practices and Prevention
Source: forbesindia.com
Staying safe in a world that’s still navigating the COVID-19 landscape means prioritizing hygiene. It’s not just about washing your hands; it’s about adopting a holistic approach to minimize your risk and protect yourself and others. Simple, consistent practices can make a significant difference.
Effective hygiene isn’t a one-size-fits-all solution, but rather a combination of practices that work together to reduce the spread of viruses like COVID-19. These practices are crucial, even as we move towards a post-pandemic world, because COVID-19, and other respiratory illnesses, are still circulating.
Effective Hygiene Practices
Maintaining good hygiene is a multi-faceted approach that includes several key elements. Consistent application of these practices significantly reduces your chances of contracting and spreading respiratory illnesses.
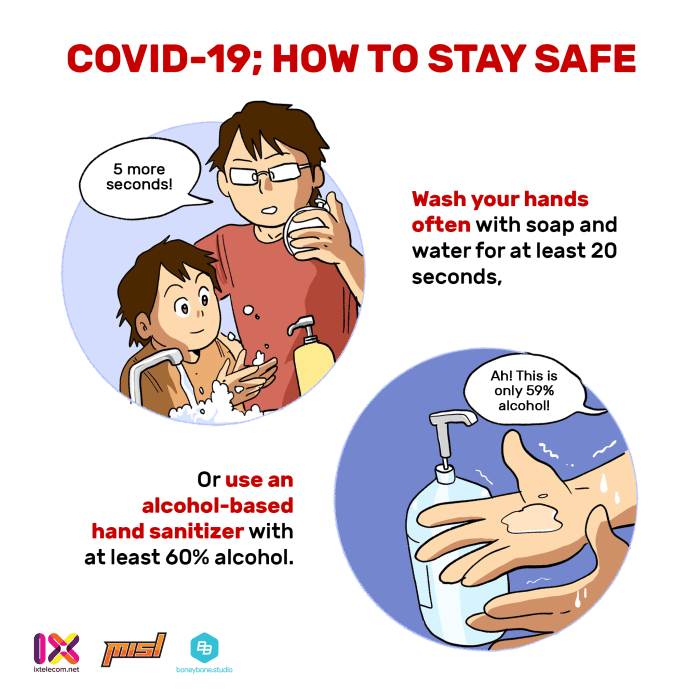
- Frequent Handwashing: Wash your hands thoroughly with soap and water for at least 20 seconds, especially after being in public spaces, before eating, after using the restroom, and after coughing or sneezing.
- Hand Sanitizer Use: When soap and water aren’t available, use a hand sanitizer containing at least 60% alcohol. Apply enough to cover all surfaces of your hands and rub them together until they are dry.
- Respiratory Etiquette: Cover your mouth and nose with a tissue or your elbow when you cough or sneeze. Dispose of used tissues immediately and wash your hands.
- Clean and Disinfect Surfaces: Regularly clean and disinfect frequently touched surfaces, such as doorknobs, light switches, and countertops, using an appropriate disinfectant.
- Avoid Touching Your Face: Minimize touching your eyes, nose, and mouth to prevent the virus from entering your body.
- Stay Home When Sick: If you’re feeling unwell, stay home to avoid spreading illness to others.
Proper Handwashing Techniques and Respiratory Etiquette
The effectiveness of handwashing hinges on proper technique. Simply wetting your hands isn’t enough. You need to thoroughly lather all surfaces, including between fingers and under nails, for at least 20 seconds – the time it takes to sing “Happy Birthday” twice. Similarly, covering your coughs and sneezes with your elbow (rather than your hands) prevents the spread of germs to surfaces you might later touch.
The Role of Mask-Wearing in Preventing the Spread of the Virus
Masks act as a barrier, reducing the expulsion of respiratory droplets into the air when an infected person coughs, sneezes, or talks. This significantly reduces the chance of infecting others. Even if you’re not infected, wearing a mask can offer some protection by reducing the amount of virus you inhale. The effectiveness varies depending on the type of mask.
COVID-19 might be fading from headlines, but it’s still out there, so keeping your distance and masking up in crowded spaces remains crucial. Even finding a peaceful hobby like birdwatching can involve some risk, so check out this guide on the best bird watching gear to ensure you’re prepared for safe, socially distanced adventures. Remember, staying healthy means being mindful, even while enjoying the great outdoors.
Comparison of Different Types of Face Masks and Their Effectiveness
Different masks offer varying levels of protection. While N95 respirators provide the highest level of filtration, they require proper fitting and are usually reserved for healthcare professionals. Surgical masks offer good protection and are widely available. Cloth masks offer less protection than surgical masks, but still provide some level of barrier protection. The effectiveness also depends on the material and number of layers.
For instance, a well-fitted N95 respirator can filter out at least 95% of airborne particles, while a simple cloth mask might only filter a smaller percentage, but it’s still better than nothing. The choice of mask depends on the level of risk and the availability of different options. During periods of high transmission, higher-level protection is recommended.
Testing and Early Detection
Early and accurate detection of COVID-19 remains crucial in controlling its spread and mitigating severe outcomes. Understanding the different testing options available and knowing when to get tested are vital steps in protecting yourself and your community. This section will clarify the types of tests, their accuracy, and the appropriate situations for testing.
Different Types of COVID-19 Tests and Their Accuracy
Types of COVID-19 Tests
COVID-19 tests primarily fall into two categories: molecular tests and antigen tests. Molecular tests, such as polymerase chain reaction (PCR) tests, detect the virus’s genetic material (RNA). These tests are highly accurate, even detecting very low viral loads, making them ideal for confirming infection. Antigen tests, on the other hand, detect specific proteins on the surface of the virus. While generally quicker and cheaper than PCR tests, antigen tests are less sensitive and may produce false negative results, particularly in the early stages of infection or when viral load is low. Rapid antigen tests are commonly used for quick screening, but a positive result should ideally be confirmed with a PCR test. The accuracy of each test can vary depending on factors like the quality of the test itself, the timing of the test relative to infection, and the expertise of the person administering the test.
Recommended Testing Situations
Testing is recommended in several scenarios. Individuals experiencing COVID-19 symptoms, such as fever, cough, shortness of breath, or loss of taste/smell, should seek testing immediately. Testing is also advisable for those who have been in close contact with someone who has tested positive for COVID-19, even if asymptomatic. Furthermore, testing may be necessary before and after travel, depending on the destination’s requirements, or for participation in certain activities or events. Regular testing might be recommended for individuals in high-risk settings, such as healthcare workers or those living in congregate settings. Pre-surgical testing may also be necessary in certain situations.
Accessing COVID-19 Testing Resources, Covid 19 isnt over how to stay safe
Access to COVID-19 testing varies depending on location and healthcare systems. Many countries have established widespread testing networks, including public health clinics, hospitals, pharmacies, and dedicated testing centers. Online resources and local health department websites usually provide information on testing locations, appointment scheduling, and available test types. Some employers may also offer on-site testing or provide resources to access testing. Private healthcare providers also offer testing services, though these may involve costs not covered by insurance.
Steps to Take After a Positive Test Result
Receiving a positive COVID-19 test result requires immediate action. First, isolate yourself from others to prevent further spread. This involves staying home and avoiding contact with others, including family members, as much as possible. Inform close contacts of your positive test result so they can monitor their health and get tested if necessary. Follow guidance from your healthcare provider or local health authorities on treatment and monitoring your symptoms. This might include rest, hydration, and over-the-counter medications to manage symptoms. Seek medical attention if your symptoms worsen or you develop severe complications. A positive test also triggers reporting requirements, which vary by jurisdiction. You will be advised on this process by your healthcare provider or local health authority.
Managing COVID-19 Risk in Daily Life
Living with COVID-19 means navigating a world where the virus is still present, albeit often at lower levels than during peak periods. This requires a proactive approach to risk management, adapting our behaviors to minimize exposure in various daily settings. Understanding your personal risk tolerance and implementing appropriate strategies is key to staying safe and healthy.
Minimizing COVID-19 Risk in Different Settings
Successfully managing COVID-19 risk involves tailoring your approach to the specific environment. The level of risk varies significantly between a well-ventilated office and a crowded indoor concert. In workplaces, maintaining good ventilation, practicing regular hand hygiene, and following any company-specific protocols are crucial. Schools might benefit from enhanced cleaning schedules, staggered break times, and promoting outdoor activities whenever possible. Social gatherings, especially those indoors and with many attendees, present a higher risk and necessitate careful consideration of individual risk factors and mitigation strategies. Think of it like this: the more people you interact with in a confined space, the higher your risk.
Checklist for Social Events
Before attending social gatherings, it’s beneficial to assess the potential risks and take proactive steps to mitigate them. This checklist provides a framework for making informed decisions.
- Assess the venue: Is it indoors or outdoors? How large is the space? What is the expected number of attendees?
- Consider the attendees: Are there any individuals at high risk present? Will there be close contact?
- Check your own health: Are you experiencing any COVID-19 symptoms? If so, stay home.
- Plan your transportation: Avoid crowded public transport if possible.
- Pack hand sanitizer and consider wearing a mask, especially in crowded or poorly ventilated areas.
The Importance of Ventilation and Air Quality
Proper ventilation significantly reduces the concentration of airborne viruses, including SARS-CoV-2. In indoor spaces, good airflow dilutes viral particles, lessening the chance of transmission. Strategies to improve ventilation include opening windows, using air purifiers with HEPA filters, and ensuring HVAC systems are properly maintained and functioning efficiently. Studies have shown a clear correlation between better ventilation and lower COVID-19 transmission rates in various settings, from classrooms to offices. Imagine a room with poor ventilation – viral particles linger in the air for longer periods, increasing the risk of infection. Conversely, a well-ventilated space allows for quicker dispersal of these particles.
Assessing and Managing Personal Risk Levels
Your personal risk level depends on several factors, including your age, underlying health conditions, vaccination status, and the level of community transmission in your area. Individuals with weakened immune systems or chronic health conditions generally face a higher risk. Staying updated on local COVID-19 case numbers and adapting your behavior accordingly is crucial. For example, during periods of high community transmission, you might choose to limit your attendance at indoor gatherings or opt for outdoor activities instead. Regular self-assessment, combined with an understanding of your personal vulnerabilities, empowers you to make informed decisions about your activities and interactions. This personalized approach to risk management allows you to prioritize your health and safety without unnecessary restrictions.
Addressing Misinformation and Building Trust
Source: ixtelecom.net
The COVID-19 pandemic wasn’t just a health crisis; it was also an infodemic. A flood of misinformation, often spread through social media and unreliable sources, created confusion and hampered efforts to control the virus. Combating this requires understanding the common misconceptions, identifying trustworthy sources, and developing critical thinking skills to navigate the digital landscape. Building trust in accurate information is paramount to protecting public health.
Misinformation surrounding COVID-19 has taken many forms, hindering effective public health responses. Understanding these misconceptions is the first step towards building a more informed and resilient community.
Common Misconceptions about COVID-19
The spread of inaccurate information about COVID-19 has had significant consequences. Many false claims have fueled hesitancy towards vaccination and preventative measures, leading to avoidable illness and death. Some prevalent misconceptions include the belief that COVID-19 is no more dangerous than the flu, that masks are ineffective, and that vaccines cause serious side effects. These beliefs, often fueled by biased or fabricated information, undermine public health initiatives and prolong the pandemic’s impact.
Credible Sources of Information Regarding COVID-19
Reliable information is crucial for making informed decisions about your health and safety during a pandemic. Relying on credible sources helps ensure you’re making choices based on facts, not fear or misinformation.
Here are some trustworthy sources for COVID-19 information:
- World Health Organization (WHO): The WHO provides up-to-date information on the pandemic, including global statistics, guidelines, and research findings.
- Centers for Disease Control and Prevention (CDC): The CDC offers comprehensive information specific to the United States, covering prevention, treatment, and data tracking.
- Your National Public Health Agency: Most countries have their own public health agency that provides tailored guidance and information relevant to their specific context.
- Reputable Medical Journals: Publications like the *New England Journal of Medicine* and the *Lancet* publish peer-reviewed research on COVID-19.
The Importance of Reliable Information Sources
Choosing reliable sources of information is critical for navigating the pandemic effectively. Misinformation can lead to dangerous behaviors, hindering efforts to control the virus’s spread and protect vulnerable populations. Reliable sources provide evidence-based information, allowing individuals to make informed decisions about their health and contribute to a safer community.
A Guide to Critically Evaluating Health Information Found Online
The internet, while a powerful tool, is also a breeding ground for misinformation. Learning to critically evaluate online health information is a vital skill for protecting yourself and others.
Always check the source’s credibility. Is it a reputable organization, a qualified expert, or a biased website?
Look for evidence-based claims. Does the information cite scientific studies or reliable data? Be wary of anecdotal evidence or unsubstantiated claims.
Consider the date of publication. Medical knowledge evolves rapidly. Ensure the information is current and hasn’t been superseded by newer research.
Be wary of sensationalized headlines or emotionally charged language. These are often used to spread misinformation.
Cross-reference information from multiple credible sources. If several reliable sources report the same information, it’s more likely to be accurate.
Final Review
Source: engineeringmanagementinstitute.org
Staying safe during the ongoing COVID-19 pandemic isn’t about living in fear, but about making informed choices. By understanding the current landscape of the virus, prioritizing vaccination and boosters, maintaining good hygiene, and staying informed, we can significantly reduce our risk and protect our communities. Remember, vigilance and responsible actions are key to navigating this evolving situation. Stay safe, stay informed, and stay healthy.

